New Beacon of Hope
Woman with metastatic breast cancer now cancer-free for two years after an experimental immunotherapy.
By Aatika H Jain
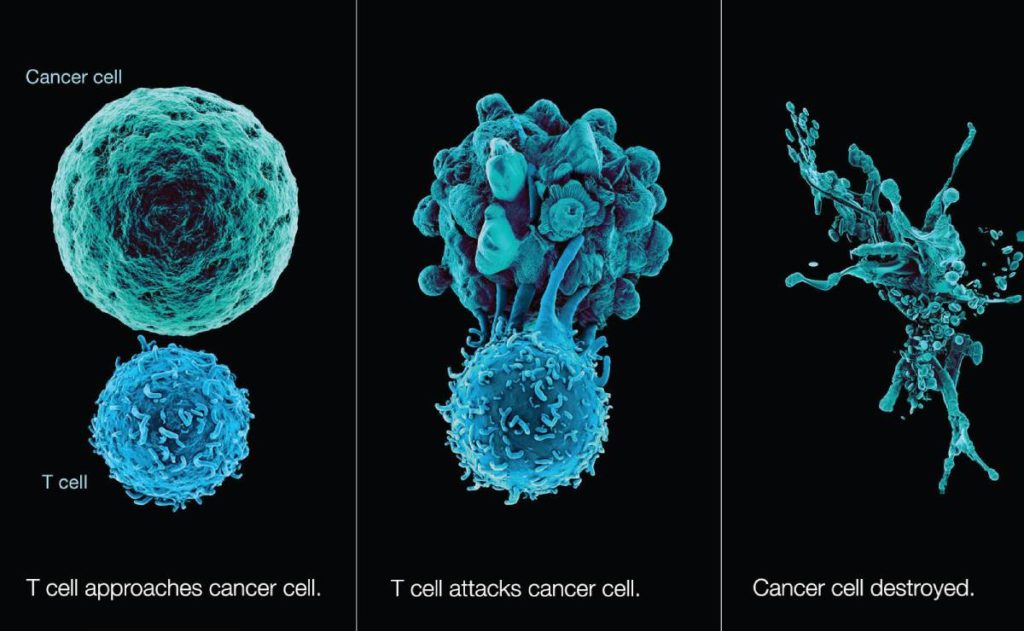
Getting the body to wage its own war against cancer is one of the most recent successes of science. In more exciting news from this area, a new kind of immunotherapy has successfully led to the total regression of metastatic breast cancer in a patient for whom other conventional treatments had not worked out. Immunotherapy is a method of treating or preventing disease by stimulating an immune system response by modifying the body’s immune cells. When immunotherapy is used for the treatment of cancer, an immune response is stimulated that will potentially recognize and destroy only the cancer cells without harming the healthy cells.
The heartening immunotherapy success is a part of phase II clinical trial going on at the National Cancer Institute (NCI), Maryland, the US, headed by Dr. Steven A Rosenberg. Published in Nature Medicine, the research illustrates the clinical trial currently underway that has completely cured a woman of advanced-stage breast cancer, which had spread to her liver too. Prior to the new therapy, Judy Perkins, 52, was given three years to live by her doctors when traditional chemotherapy couldn’t help kill the tumor cells. Two years hence, she is still free of cancer.
Dr. Peush Bajpai
Senior Consultant Medical Oncologist, Manipal Hospital, New Delhi
“Immunotherapy, approved by FDA and practiced worldwide, is Immune Checkpoint Inhibitors. It is effective in nearly 30- 40% of patients with advanced metastatic cancers,” explains Dr. Peush Bajpai, Senior Consultant Medical Oncologist, Manipal Hospital, New Delhi. Immunotherapy has previously been successful in beating non-Hodgkin’s lymphoma and metastatic melanoma and has been in use against advanced stages of cancer, including lung cancer and prostate cancer. The new immunotherapy approach administered by the NCI team was based on adoptive cell transfer (ACT), which boasts a particular type of immune cell called T cells to target and kill tumors. The team studied the genetic mutations in the cancerous cells specific to the patient and also identified tumor-infiltrating lymphocytes (TILS) that could recognize four of the 62 discovered mutations. These TILS were grown in large numbers in the lab and later infused back into the patient’s body.
The ABCs of Immunotherapy
Cells in the human body become cancerous when they start growing out of control and the immune system does not recognize them as foreign, either because they do not look different from the normal cells or the cancer cells release substances to inhibit the immune system. Immunotherapy stimulates the immune system to recognize the cancer cells and boosts its capacity to destroy them efficaciously.
Also called biologic therapy, immunotherapy has been successful in treating certain kinds of malignancies for the past few decades. New approaches have been under trial to cure more types. Cancer immunotherapy has come a long way since the use of Coley’s toxin in the early 20th century. Dr. William B Coley, called the Father of Immunotherapy, was the first to utilize a person’s immune system to cure cancer. In the late 19th century, he successfully administered bacterial antigens to induce a reaction against malignant cancer such as sarcoma, lymphoma, and testicular carcinoma. But his results could not be replicated by other doctors.
The risk of fatal side effects of this therapy and the lack of knowledge of the actual mechanism of Coley’s toxin led to radiotherapy and surgery being adopted as the conventional treatment for cancer in the early 20th century. Thomas and Burnet first propounded the immune surveillance theory that lymphocytes kept a check on mutated somatic cells. This gave a boost to the immunotherapy approach to treat cancer. Milstein and Köhler made monoclonal antibodies in the lab for the first time in the 1970s and in 1997, the first monoclonal antibody was approved for treatment of non-Hodgkin’s lymphoma.

In 1976, attenuated bacterial antigens were again used to cure cancer. BCG (Bacille Calmette-Guérin), the tuberculosis vaccine, was administered in a trial to stop bladder cancer from recurring. It worked well and is still used to treat bladder cancer. Different types of immunotherapy are in use to fight cancer. Monoclonal antibodies (MABs) are lab-produced immune proteins. They are used in targeted therapy as well as immunotherapy.
For example, they are used as angiogenesis inhibitors in targeted therapy to prevent cancerous cells from forming new blood vessels, thus inhibiting their growth. Some MABs in immunotherapy stick to particular proteins on the cancerous cells so that the immune system can identify and destroy them.
Immune checkpoint inhibitor is a type of MAB used to block the protein released by cancerous cells, which prevents the immune system from destroying them in targeted therapy. They are used in the treatment of melanoma and lung cancer. Cancer vaccines (prevention and treatment vaccines) are being used both as a prevention as well as a treatment method. They might slow down or stop the cancer growth, prevent relapse or kill the remaining cancerous cells, if any, after other treatments. Cytokines are naturally occurring proteins that improve the human immune system. Interferon and interleukin are cytokines that have been developed in the lab and are being used for cancer treatment. The promising success in the case of Judy Perkins has excited the cancer community but Dr. Rosenberg says the research is only in the experimental stage. However, this new approach doesn’t depend on the type of cancer but the mutations. So it could guide the specialists in the treatments of many cancer types.
Various insurance schemes and central government health programmes cover Immunotherapy in India now. This has improved the use of the procedure as it is a high cost one at present.
“Immunotherapy not only scores better where the quality of life issues are concerned but also provides better survival rate in comparison to chemotherapy,” says Dr. Bajpai. “I remember a patient who was exposed to immune checkpoint inhibitor in a Stage 4 carcinoma lung where a median survival with chemotherapy was 18 months. It has been 3 years since he got immunotherapy and he continues to be clear of his disease process.” When using immunotherapy for cancer, one of the challenges is identifying effective biomarkers, and to find cases where they would work best, he says. Various insurance schemes and central government health programmes cover immunotherapy in India now. This has improved the use of the procedure as it is a high cost one at present. For immunotherapy to become a more viable option for cancer treatment, the results need to be improved along with bringing down the cost. “The possible options are either combination of two immunotherapeutic agents or an enzyme inhibitor like PARP in combination with immunotherapy,” says Dr. Bajpai. “A possible immunogram of the tumor could also be a biomarker of the future.”