The Gift Of Life

Oncofertility treatment ensures that young people battling cancer do not miss out on the chance to become parents later in life
By Anila Mathew Vivek
Cancer can play havoc with life. Right from the shocking diagnosis to the emotionally and physically exhausting rounds of therapy, the journey of recuperation is fraught with problems. Amid dealing with a life-threatening illness, handling the finances, suffering the side effects of treatment and clinging on for dear life, the dreams of having babies takes a backseat. However, with increasing incidences of cancer and higher survival chances combined with the time factor i.e. the disease striking at a much younger age, the field of oncofertility has become very significant. This is a cross-disciplinary area of medicine and research that deals with fertility preservation among cancer patients. Cancer treatments haven’t really improved with regard to side effects. Chemotherapy and radiation therapy adversely affect the fertility of women and men. The drugs used in treating cancer can also bring about early menopause, thus preventing any chance of giving birth to a child. There are options like surrogacy and adoption for women who cannot conceive after a bout of cancer. However, oncofertility can help women realise their dream of giving birth to their child naturally through cryopreservation. The various options available include freezing the egg, embryos or ovarian tissue, ovarian suppression and ovarian transposition. Oocyte cryopreservation or freezing eggs is a joint effort between an oncologist, an endocrinologist, an anaesthesiologist and an infertility specialist. Also known as egg banking, the process involves removing mature eggs and freezing them. The frozen eggs can later be thawed, fertilised with sperm and then implanted in the uterus.
The process of collecting eggs can be done in any IVF facility, keeping in consideration the patient’s menstrual cycle. Hormonal injections are administered to ensure simultaneous development of several eggs in the ovaries. The eggs are then collected during outpatient surgery when an ultrasound is used to guide a needle through the upper part of the vagina and into the ovary to collect the eggs (ova). Earlier, embryo preservation was the procedure followed, where a male partner was also required to donate sperm. But, in cases of separation or divorce, women could not lay claim to the frozen embryos, as the legal rights would reside with the father. However, egg banking can be done regardless of marital status now and women can access their eggs whenever they are ready for motherhood. This method can be unsuitable in certain cases such as the discovery of cancer at an advanced stage. Treatment will have to begin immediately and three weeks cannot be spared for collecting eggs. In other cases, the medicines used for induction of ovulation may have an adverse effect on cancers.
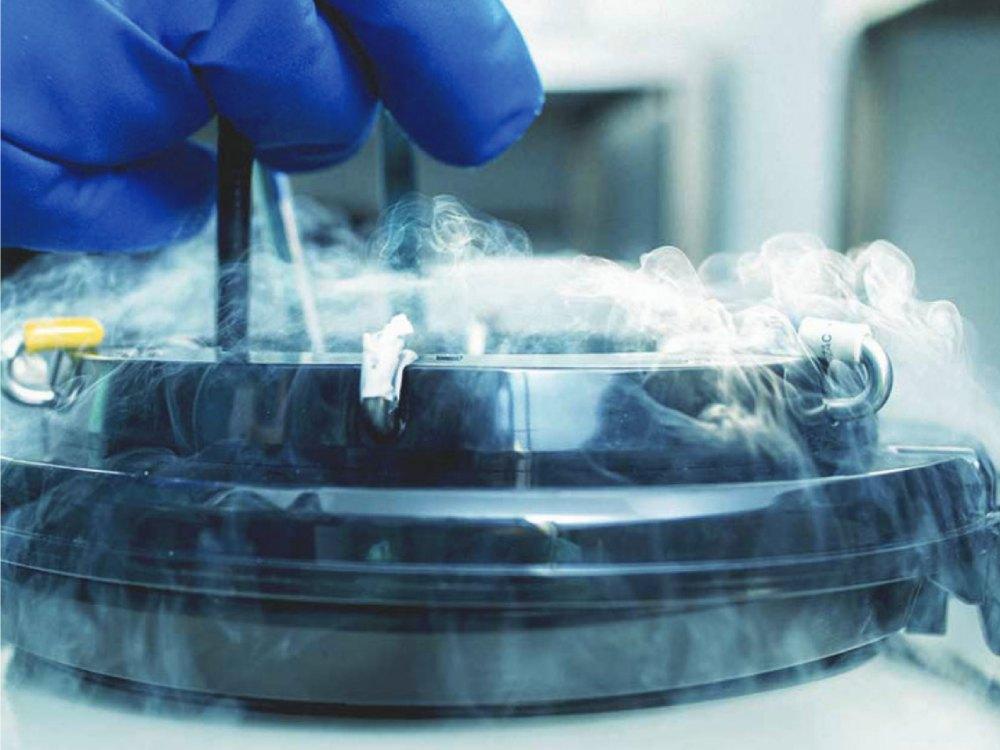
Rich in the oestrogen hormone, the injections may aggravate certain kinds of cancer like breast cancer. Egg freezing has been more difficult than freezing embryos, since the egg is the largest cell in the human body that has a lot of water. This leads to formation of ice crystals that can damage the egg. However, a new method called vitrification has increased the efficacy of egg banking. There have been successful results in developed countries. In India, there are emotional, legal, religious and financial implications that often prevent women from making such an informed choice. There is not much awareness about such an option, but all IVF centers provide facilities for the innovative procedure at a relatively affordable rate. An annual fee will have to be paid to keep the eggs preserved. Says gynecological oncologist Neha Bhargava: “Awareness is very important. The decision, I think, should be left to the patient. But every oncosurgeon, every onco-gynaecologist should tell the patient about their options. Doctors have a major role to play here, to make the patient aware that she can still have a baby. It is also not just about having a baby. The anti-cancer drugs also cause premature ovarian failure, causing menopause much earlier. So I think every girl should get this right of preserving her sexuality and ovarian function.” She also emphasises that both men and women who are getting treated for cancer should be made aware of cryopreservation.

“DOCTORS HAVE A MAJOR ROLE TO PLAY HERE, TO MAKE THE PATIENT AWARE THAT SHE CAN STILL HAVE A BABY. IT IS ALSO NOT JUST ABOUT HAVING A BABY. ANTI-CANCER DRUGS CAUSE PREMATURE OVARIAN FAILURE, CAUSING MENOPAUSE MUCH EARLIER. SO I THINK EVERY GIRL SHOULD GET THIS RIGHT OF PRESERVING HER SEXUALITY AND OVARIAN FUNCTION.”
Dr Neha Bhargava – Gynecological Oncologist