Reality Check

This month’s column takes a look at unrealistic expectations in oncology and how these can be tackled.
Patients, especially those suffering from cancer, look to their doctors and specialists for hope and succour. However, sometimes they can come with the burden of unrealistic expectations.
What is the meaning of unrealistic expectations?
‘Expectation’ refers to a strong belief about something that is likely to occur in the future, usually something good. ‘Unrealistic’ essentially refers to the remote likelihood of it becoming reality. It, therefore, translates, into the failure to face the truth. This is not uncommon when faced with a difficult situation, especially if it is unexpected.
Other words that can describe it are impractical, improbable and unworkable. In short, when someone wants the future to hold a good outcome which is unlikely to happen, it translates to unrealistic expectations. Because it is a perception, a state of mind, its exact nature and specifics vary from person to person. It is something that exists within and is, therefore, very difficult to be ascertained by the opposite party. It is based on a combination of intellectual, rational, spiritual and traditional perceptions.
Perception is a state of mind. In my 30 years of experience, I have seen it vary from patient to patient. Unrealistic expectations do not correlate with education. Some of the most educated patients have significant unrealistic expectations whereas the illiterate often accept the situation in an insightful manner.
Dr. Govind Babu, Bengaluru

Common unrealistic expectations
a) At initial diagnosis: Some patients are not willing to accept that they have cancer. Common statements include the following:
i. Doctor, this biopsy tissue must have been exchanged with someone else’s. This diagnosis is wrong. I want the biopsy to be repeated.
ii. I do not believe this report. I want to show the biopsy slide to Dr. X in Mumbai.
iii. How can I have cancer? I never drink or smoke. I only eat homecooked food.
iv. I am feeling totally fine. I am able to do all my work. I have no symptoms. There must be some mistake. Doctor, please check me once more.
b) During therapy: Some patients will be more concerned with things other than their cancer.
i. Doctor, I am losing my hair. I cannot go to my kitty party. I don’t want any treatment that will lead to hair loss.
ii. You had told me that you will give me medicines to prevent vomiting. Why did you not give them to me? I have nausea just at the sight of food. How can I eat anything?
iii. I was given the discharge card specifying that the next dose is today. Now you are telling me that my blood reports are not satisfactory and I have to wait for three days before the next dose. But I have scheduled a trip at that time.
c) After completion of therapy: the problem does not get over when the cancer-directed therapy is over.
i. Now that my treatment is over, I am totally cured and do not have to come for follow up, right?
ii. My hair has come back. But it is different. How come it is of a different color now?
iii. You keep asking for blood tests and scans at regular intervals. But they are all normal. Why should I continue doing them?
d) During disease recurrence: during this stage, patients and families are generally upset and very concerned. Often this gets converted into blaming their doctor.
i. But, doctor, you had guaranteed that cancer would never come back.
ii. How is it that the cancer is back? I was following your instructions and doing regular checkups and tests.
iii. The cancer is back because you did not give me proper instructions on what to eat and what not to eat.
e) At the end of life care: here we commonly face two extremes of reactions from families.
i. We are not willing to accept that nothing can be done to stop cancer from growing. We are willing to try anything even if the chance of response is less than 1 percent.
ii. We know that our patient is terminally ill. However, we do not want to give him morphine for pain control. We do not want him to get addicted to such substances.
Unrealistic expectations among our patients are seen almost on a daily basis. When discussing with my colleagues, I have realised that they are facing a similar situation. The classic case is as follows. We patiently explain the details of the disease including its nature, outcome and financial issues. After counseling for 30 minutes, the usual response is, “Doctor we understand all this, but do you guarantee 100% cure?” This is really frustrating because it affects the doctor-patient relationship in a negative way. Patients and families keep on taking second, third and fourth opinions, each time seeking a guaranteed response, something that no doctor can provide.
Dr Sumant Gupta, Faridabad

A global phenomenon
The phenomenon of unrealistic expectations is not limited to one ethnic, social or geographic group. It is universal. It exists all over the world. It pervades all strata of society. The lay press (Reuters) and scientific medical oncology publications of the highest standards (New England Journal of Medicine, Journal of Clinical Oncology) have ample evidence of its widespread existence. In the USA, for instance, Cancer Care Outcomes Research and Surveillance (CanCORS) was a huge multi-center consortium study that was funded by the National Cancer Institute (government).
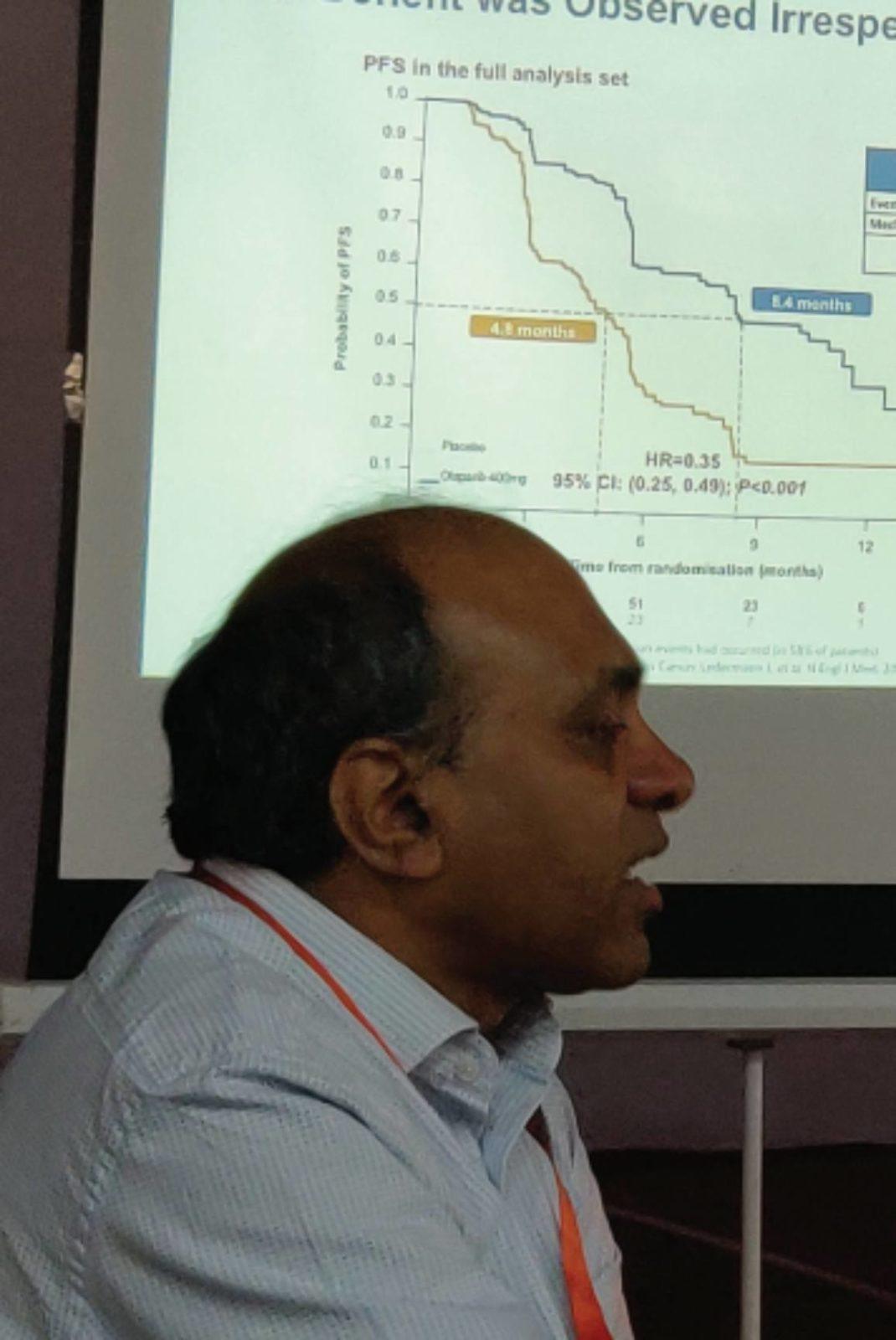
One study was on colorectal cancer and the other was on lung cancer. (Ref: https:// sciencebasedmedicine.org/ expectations-versus-reality-in science- based-oncology/https:// sciencebasedmedicine.org/ expectations-versus-reality-in science- based-oncology) Both patients and their oncologists were asked specific questions to find out about the quality of cancer care planned and/ or received. All patients were at advanced stages where the intent of treatment was palliative (cure not possible). The NEJM study included 1,193 cases whereas the JCO study involved 384 patients. For those receiving chemotherapy, the assessment was done among newly diagnosed patients with stage IV (metastatic) lung or colorectal cancer, four months after starting chemotherapy. For those planning for palliative radiation therapy, the assessment involved newly diagnosed lung cancer, stage IV and/or stage IIIB (due to malignant pleural effusion).
Three simple questions were asked:
Will your treatment help you live longer?
Will your treatment cure your cancer?
Will your treatment help you with problems you are having because of your cancer
Surprisingly, the answers of the majority of patients receiving chemotherapy (69 percent with lung cancer; 81 percent with colorectal cancer) indicated that they had not accepted that their disease could not be cured. Interestingly, this response was higher among patients of Asian ethnicity (odds ratio of 4.32). Even for radiation therapy, the majority of patients did not accept the incurable nature of their illness (seen in answers received from 64 percent of cases).
Very important was the fact that if the patients had inaccurate beliefs about one mode of therapy, they also had the same unrealistic expectations of cure with the other mode of therapy; 92 percent of patients with inaccurate beliefs about the benefit of chemotherapy also had inaccurate beliefs about the response to RT. This is an important insight. Even when the same patient is counseled by different oncologists (medical and radiation oncologists), the false belief regarding the chance of cure still persists.
Unrealistic expectations are not limited to cure and survival alone. It also affects the cosmetic outcome. This has been well documented in patients with breast cancer. Last year, we saw how patient expectations varied both after mastectomy as well as after breast conservative surgery (https://www.deccanchronicle.com/lifestyle/health-andwellbeing/020318/breast-cancerpatients-may-have-unrealisticexpectations-from-mastecto.html). This survey included 96 women having breast cancer and was published in JAMA. They were studied before surgery and one year after surgery. Patients who opted for mastectomy underestimated their satisfaction after opting out of reconstruction. Even the patients who went for breast reconstruction were dissatisfied with the results with respect to the feeling of sexual attractiveness.
While sharing the right picture of the disease, we have to balance it with preserving hope. It is a delicate balance. When the patient sheds his inhibitions and asks their inner doubts, our job becomes easier.
Dr. Purvish Parikh, Mumbai

Why this occurs
When faced with the diagnosis of cancer, patients are under stress and very anxious. They have to come to terms with their diagnosis as well as try to comprehend the medical jargon. Under the circumstances, there is a significant chance of misunderstanding regarding their specific type of cancer, overestimating their chance of a positive outcome and focusing only on that part of the doctor’s counseling that they want to hear—resulting in unrealistic expectations from their anticancer treatments. This is not uncommon when the discussion is about a lack of a cure, and palliative end-of-life care.
Imagine the anguish the terminally-ill cancer patient faces. He does not want to acknowledge that he will shortly cease to exist on this earth. He does not face the end of his existence. He cannot cope with the thoughts of pain, suffering, and the loss of self-esteem. The ‘natural’ reaction is denial—to deny that they are dying even when their oncologist tells them that they cannot be cured.

Thomas J Smith and Dan L Longo have written eloquently regarding these aspects in their editorial in the NEJM entitled, Talking to Patients about Dying. Even when they understand the prognosis, patients often want to clutch at straws and anything that might have a positive benefit becomes the focus of attention. As we have seen often in Indian patients, previous studies from the west have also shown that patients with advanced cancer would accept toxic treatment for even a 1 percent chance of cure.
Patients, therefore, end up selecting long-course therapies that are often futile, at the expense of quality of life. Thus, unrealistic expectations are misunderstandings that represent an important obstacle to planning palliative as well as end-of-life care. In other words, this disconnect between the science-based goals of treatment explained by the doctor and what patients perceive in their mind as the goals of treatment is a wide chasm. And because it is in the patient’s mind, it is not possible for others to recognize it. In North America, the problem is compounded by misleading advertising.
Open any TV channel and viewers are bombarded by new treatment medications/ methods. Direct-to-patient advertisements often say, if you are suffering from XXX ask your doctor if YYY is applicable to you. No wonder patients have already made up their minds what is of benefit to them and go to their specialist demanding the latest medication. The situation in New Zealand is no different. In a survey of almost 1,000 patients, Hudson and colleagues found overestimation of benefits even for cancer screening and chemo-preventive medications for healthy people or those with high-risk behavior. The role of quacks and self-styled “cancer doctors” cannot be underestimated. They treat patients with magical remedies, promise miracles and cleverly cover up when cancer starts progressing.
Patients have often shared some misleading statements made to them by quacks. For example, “the tumor will swell before it disappears” and “cyst formation means that the tumor is dying inside“. Hope is also universal. We all live on hope—of a better life, a better future. In patients, this results in the expectation of a positive outcome despite the circumstances. Hope transcends reality. It is also a dynamic, limbic, and necessary response to the threat of cancer. For doctors and oncologists, one of the tasks is to never take away hope from patients. Remember the “placebo” effect of sugar pills. Hope therefore plays an important role in improving quality of life.
The final goal should be to convert hope into a positive acceptance of what is inevitable. Hope has been shown to increase when the patient is provided up to‐ date treatment information; their oncologist comes across as knowledgeable about their cancer and being comforted that any pain shall be controlled. Occasional use of judicious humor and sincere expression that they will not be abandoned are also beneficial. Finally, we have to accept that some patients shall continue to hold false expectations even when a realistic prognosis has been clearly discussed. This is because denial is a well-recognized coping mechanism, with about 10 percent of patients choosing not to believe in their terminal status and finite life expectancy.

A diagnosis of cancer can be overwhelming news even for the brave of heart. In addition to an emotional component clouding one’s comprehension of the initial discussion with one’s physician, the subsequent information overload as one turns to Dr Google can make it difficult to parse the chaff from the grain. It is remarkable that in an era when we are talking about 5G speeds and Artificial Intelligence, there is a paucity of reliable online resources that patients can turn to for education and navigation. Filling this lacuna may help diminish the problem of heightened expectations.
Dr Ravi Vij St Louis, USA
Role of well-meaning friends and social media
The patient, faced with a new diagnosis of cancer or news that it is progressing/has come back, is already under tremendous duress. He is also vulnerable to the influences of family and friends. Well-meaning recommendations based on anecdotes or faintly remembered past conversations suddenly gain undue importance. On top of this, there is easy access to social media and the Internet, which is full of conflicting advice. Caregivers with the greatest influence or the head of the household have to shepherd the patient wisely and patiently. Without the skills of the professional counselor, their task is daunting and full of pitfalls. In cancer, there is a window of opportunity to optimize treatment. This is often lost while the family debates on the best way forward. Postponing the decision is like taking the decision not to do anything. This is the biggest threat faced by cancer patients.
Counseling sessions
Cancer patients and their families should take counseling sessions seriously. The family must designate one person to be their spokesperson. He/she should preferably be the primary caregiver, who will be present at all crucial moments and also be in a position to take decisions on behalf of the family. This is the only way miscommunications can be avoided. In India, in most instances, there are at least two camps, the family of the patient and the family of his/her spouse. Each of them is suspicious of the other and sometimes insists on separate counseling sessions. In addition, there are some self-proclaimed representatives who demand to know what is going on in full detail but disappear when the patient really requires their help.
Both the patient’s family as well as healthcare providers need to understand that each other’s time is valuable and should not be misused. The patient’s team should come to counseling sessions well prepared with their questions, preferably written down. The session should not be converted into a test about the healthcare teams’ competence or knowledge. So also the healthcare team should provide the real picture and also answer all questions crisply and clearly, avoiding medical jargon. This is especially required during end-of-life situations. Here it can improve mental quality of life for the cancer patient as well as prepare caregivers with coping skills to prevent psychiatric complications during bereavement.

Since 2006, the Institute of Medicine has led the interest in the development of a systematic Cancer Survivorship Care Plan (SCP) to mitigate the risk of ‘Unrealistic Expectations’(https://www.medscape.com/viewarticle/892920) . This was with the aim of targeting the specific problems that a cancer survivor can face. The idea was that each and every cancer patient should receive an individualized SCP once the cancer-directed treatment is about to end. Unfortunately, they were found to be ineffective in improving outcomes in cancer patients. No wonder this fell into disrepute.
Even in the USA, with its abundant resources, only a limited number of professionals follow it; 43 percent of NCI-designated cancer centers, 20 percent of academic oncologists and only a handful of those practicing in the community. The only potential advantage from 13 randomised and 11 nonrandomised trials was that such SCPs improved the adherence to screening for potential cardiomyopathy. Hence, wasting time and resources on SCP is no longer recommended.
Patients’ expectations can be addressed in a collaborative manner. This requires frank inputs from the patient as well. We cannot continue the discussion in a meaningful manner in a vacuum. Keeping in mind the paradoxical fact about communication versus understanding, we strive to provide understanding and insight using crisp and nontechnical words.
Dr. Prasad Narayanan, Bengaluru

What oncologists do
Doctors face the challenge of deciding how to manage expectations from patients and their families. For instance, doing a blood test (PSA) for screening for prostate cancer is well recognized and popular among the general public. Now if their oncologist wants to confront this by discussing recent evidence questioning its validity, the patients and families become suspicious about their doctor’s knowledge and motives. In other words, any attempt at discussing realistic expectations regarding risk, benefit and the possible outcome is interpreted as being insensitive to the needs of the patient, discrimination, failure to provide the latest treatment and threatening patients’ right (authority) to select the treatment of their choice. Social media also poses a challenge, especially when some cancer-related perception or anecdotal experience goes viral, with distorted and misleading messages.
With this background, let us discuss a paradoxical fact. All of us will be surprised to note that patients were more likely to have a correct perception about their prognosis and future, provided they also reported lower scores for physician communication. Believe it or not, but an effective communicator (receiving a high communication score from his patient) is associated with lower understanding and a higher risk of unrealistic expectations. So please keep in mind that the quality of care does not correlate with patient satisfaction scores. Doctors need only focus on being truthful and providing an accurate picture in a manner that does not increase anxiety or depression—a patient-centric approach.
While the communication style affects how each patient perceives this experience, it is the patient’s personality that actually has a major role to play in how he/ she shall react. This is the crucial unknown piece that varies from patient to patient. It is, therefore, the role of the family caregiver to give this feedback to the healthcare team. Only then can the message be conveyed by the oncologists to the patient without the development of unrealistic expectations.
Patients should declare their expectations
Patients have different goals in life. So also patients will have different goals from their cancer treatment. Unless they express the same to their oncologists, their treatment cannot be planned to suit their needs. Patients need to participate actively in the decision-making process by clearly indicating what they wish to achieve from their treatment. Some patients would like to have the best chance of cure, irrespective of cost (money, time, toxicity, convenience). Others might prefer treatment that has the least amount of side effects. Still, others might want a convenient schedule with less frequent visits required to suit the requirements of their primary caregivers. All of these are important. Unfortunately, if hidden from their healthcare team, this will lead to unrealistic expectations.
We strive tirelessly to ensure that our patients get the best treatment possible. However, the final outcome is not in our hands. We are equally upset when one of our patients does not do as well as expected. Sometimes the biological behaviour of the cancer is a puzzle that cannot be solved. Even then, we continue to offer our services and modify the treatment plan to suit the change. We are constantly on the job.
Dr Bhavesh Parekh, Ahmedabad
Doctors should declare the intent of treatment
Just as the patients should share their preferences, the oncologists should also clearly state the broad objective of the treatment and the cancer-directed care plan. Is the patient being recommended aggressive treatment with potential curative intent? Is he in a stage where cure is not likely to be achieved and treatment is with palliative intent? Will his symptoms be alleviated? Are the status of end-of-life and no cancer-directed treatment is being recommended? Is pain control the main objective? Such clarity might seem harsh at first look, but is beneficial in the long run and avoids unrealistic expectations.
Patients should understand that there cannot be any guarantee
On the internet, you might find a post, dated 28th May 2012, from the daughter of a patient with lung cancer in the USA. She laments about the rose-tinted counseling that she recalled. Instead of minimal side effects, her father had to go through an “awful time through treatment”. Instead of response to chemotherapy, her father’s disease progressed over 2 chemo protocols. Instead of having pain not related to cancer, she found that her father had bony metastasis. She felt that she had been given false hope. She felt that well-meaning optimism was misleading.
Steven Woolf from the Department of Family Medicine, Virginia, USA, says (The Price of False Beliefs: Unrealistic Expectations as a Contributor to the Health Care Crisis; swoolf@ vcu.edu) that the US spends a massive $2.6 trillion per year on healthcare. At the same time, a lot of patients are outside the safety net. A growing proportion of Americans are now foregoing health care to pay for other household needs or are facing bankruptcy (something similar to the Indian scenario).
Oncologists can use their knowledge and experience to offer appropriate and optimal cancer treatment plans personalized for each individual patient. After that, it is beyond their control. Patients must understand that answers may not exist for all their queries. Why did this cancer occur in me? Why am I not responding as well as someone else? Why did my disease come back? Why did I have this side effect? When faced with such questions, the oncologist and the healthcare team can only empathize with the patient. No one can guarantee a cure, response, absence of toxicity or no risk of recurrence. The bigger the fears, the more unrealistic the expectations. The patient and the family need to work together to understand and accept reality. This is the only way of moving forward
Also read about