TAKING THE PAIN AWAY

“You matter because you’re you, and you matter to the end of your life. We will do all we can not only to help you die peacefully, but also to live until you die.”
Dame Cicely Saunders
Founder of the palliative care movement
Death is a spectre that frightens the most sophisticated among us. This is why the mere mention of the words ‘palliative care’ brings on a panic-based response in most patients and their families.
The thought that palliative care is for the dying is a misconception, which exists due to lack of awareness; this also keeps many patients who could potentially benefit from palliative care away from its soothing support. “The mindset of people has to change,” says Dr. Boby Sarah Thomas, radiation oncologist and founder of Cancare Home Healthcare Services, Kochi, Kerala. “Rather than as a last resort, palliative care must be incorporated into the treatment regimen as early as possible to improve quality of life. The availability and accessibility of palliative care services must be increased.”
In fact, though India stood at a miserable 67th ranking in the list of 80 countries in The Economist’s Quality of Death Index 2015, Kerala was the only state that stood out with its extraordinary commitment to providing effective palliative care to the needy. To quote Padma Shri Dr. M R Rajagopal, who is titled the Father of Palliative Care in India: “There are more than 300 palliative care centers delivering services through home care, outpatient and inpatient service in India. More than 75 percent of these centers are in Kerala.
In addition, every one of the 900-plus primary health centers in the state has at least one nurse trained in palliative care.” Dr. Rajagopal is the Chairman of Pallium India, as well as a founding member of the Institute of Palliative Medicine (IPM), Kozhikode, Kerala. IPM, featured in detail in pages to follow, is the first World Health Organization Collaborating Centre for Community Participation in Palliative Care and Long Term Care in a developing country.
The ‘Kerala model’ of palliative healthcare is one that is receiving global attention because of its unique perspective on involving the community and being predominantly home-based, rather than hospice based. The state is a palliative care demonstration site for WHO and sees a large number of foreign visitors who wish to study the Kerala model for its efficacy. Kerala was the first state in the country to set a palliative care policy in 2008, followed by Maharashtra and Karnataka. And as a result of the combined efforts of all these states striving to make a difference, the National Palliative Care Strategy was formulated recently in 2012.
What is Palliative Care?
Contrary to the misconception that palliative care is treatment delivered solely to a dying patient, it is actually a specialized form of medical care for people dealing with critical illnesses, like cancer, kidney disease, and heart disease, among others. While end-of-life care is an important aspect, palliative care can in no way be restricted to that alone. Care for a patient in their final days is a small but vital component of palliative care, known as hospice care.

To die with dignity
On March 9, a five-judge bench of the Supreme Court gave legal sanction for the right to die, also allowing patients to create ‘living wills’ that, in effect, permit people to opt for passive euthanasia in case they enter a medically-irreversible coma.
Passive euthanasia involves the withdrawal of medical treatment in order to intentionally hasten the death of a terminally-ill patient. The five-judge bench reached a unanimous decision on this point and said its directives would remain in force until the Centre brought legislation in place for the same.
WHO defines palliative care as “an approach that improves the quality of life of patients and their families facing the problems associated with a life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychosocial, and spiritual.”
As its definition implies, palliative care requires a multi-pronged approach that embraces both patients and their families. Hence, such care is ideally delivered by a dedicated, multidisciplinary team comprising doctors, nurses, counselors, and caregivers. They work hand in hand to provide that extra, much-needed layer of support to the patient and their family. Palliative care looks beneath the surface and improves the quality of life of the patient and their family in a holistic manner. The earlier palliative care is introduced in the course of a progressive, chronic illness, the better the quality of life for a patient and his/her family.
Around the World
Dealing with a serious illness can take a toll on both the patient and their family, making palliative care an extreme necessity. However, unavailability and unaffordability of proper care are as much a matter of concern as the lack of awareness. This lack of access is a global concern, and immediate action to spread its reach and make it affordable for all is imperative. Even though palliative care is an element of universal health coverage under the WHO, it has largely been ignored.
In October 2017, The Lancet Commission on Global Access to Palliative Care and Pain Relief published a study, which spanned two and a half years, to delve into the scenario. The commission studied the care provided to people suffering from any of the twenty most serious conditions—including cancer, malnutrition, lung disease, Alzheimer’s, HIV, tuberculosis, and trauma injuries among others—in 172 countries. The final report described a wide and deep abyss in access to painkillers between rich and poor countries.
Globally, millions of people who die each year of chronic illnesses could have had a better quality of life in their time, only if low-cost pain drugs were available to provide palliative care. Without a doubt, the culprit here is the high cost of drugs in low-income countries. Further, around 83 percent of the 61 million people who suffer from chronic illnesses annually worldwide live in low and middle-income countries, where there is little or no access to adequate palliative care methods.
According to the report, where a pain relief drug costs 3 cents per 10mg dose in high-income countries, the same drug costs more than fivefold in low-income countries. What’s more shocking is that the US produces and imports more than 30 times as much narcotic pain relievers than it needs. In contrast, countries like Haiti and Nigeria receive only less than one percent of their needs. A country worthy of mention here is Uganda; though only 11 percent of Ugandans needing morphine for palliative care receive it, the country is above the worldwide average. Uganda implemented an innovative solution to alleviate their access and affordability problem through initiating a government-supervised private charity that produces liquid morphine for the country’s needs.
Over the last decade, the groundwork has been laid to make the availability of pain relief and palliative care a reality for the ones in need.
It is a saddening fact that even large countries with thriving pharmaceutical industries are unable to meet their country’s needs for pain relief and palliative care. India and Indonesia supply only 4 percent of their needs, and Russia, 8 percent. China, the most populous country in the world, stands at 16 percent, beating Uganda by a small margin. The pain gap is a global health emergency that must be addressed immediately. Denying it would mean a moral and ethical failure of the medical field.
To quote Felicia Knaul, Professor, University of Miami Miller School of Medicine, “We can ensure that the 61 million people who need palliative care annually, get it. The alternative is both unacceptable and unthinkable.” Over the last decade, the groundwork has been laid to make the availability of pain relief and palliative care a reality to the ones in need. What calls for immediate action next is the need to widen the reach and better the procedures.
Where does India stand?
For a healthcare method that has existed in the country for almost 20 years, palliative care has had little coverage in the past. “Palliative care has not gained the importance it deserves here,” says Dr. Rajagopal. “Sadly, in India, we only look at the disease and entirely ignore the person. What we need is not just disease-centric treatment but an individualistic-family centered approach to treating a person. The need for palliative care is greater in India than in the West simply because the disease-specific treatment does not reach patients adequately or early enough.
In India, it is estimated that 60 percent of the people dying annually will suffer from prolonged advanced illnesses and more than 60 patients will die from cancer and in pain every hour. At present, less than one percent of the needy have access to palliative care. One percent of 10 million of the needy is indeed a large number, but we need the percentage to increase.” Of late, as Indian healthcare providers move towards a more people-centered care approach, most medical entities have embraced palliative care as a crucial aspect of patient treatment. Apart from a steady increase in the number of doctors, nurses, physiotherapists and psychologists taking up palliative care, the field has also seen active participation from carers, social workers, volunteers, and spiritual leaders.
In India, it is estimated that 60 per cent of the people dying annually will suffer from prolonged advanced illnesses and more than 60 patients will die from cancer and in pain every hour.

India’s first official nod to palliative care is a serious, vital concern that happened when the Centre modified its National Cancer Control Programme in 1984 to include pain relief as one of the elementary needs that needed to be addressed at primary healthcare centers. The pain and palliative care center, set up at the Gujarat Cancer and Research Institute in the 80s, was one of the earliest such centers that focused solely on providing pain relief.
The Indian Association of Palliative Care was formed in 1993 and became a formal body by registering as a trust in 1994. Some of the other institutions that helped give palliative care an early start in India include the Shanti Avedna Ashram, Mumbai, Regional Cancer Centre, Thiruvananthapuram, the Kidwai Memorial Institute of Oncology, Bengaluru, and the Cipla Palliative Care & Training Centre, Warje, Pune.
In addition to these institutes, there are a number of palliative care NGOs that are bringing succor and care to patients across the country, like Delhi-based CanSupport, started by social activist and cancer survivor Harmala Gupta. The largest provider of home-based palliative care in India, the organization, which was begun in 1996 with a single team and six patients, now serves nearly 2,000 patients. CanSupport also extends daycare centers that offer age-appropriate care and recreational facilities. “As a survivor, I felt obligated to play my role in ensuring that cancer patients and their families got timely support so they could make the right choices,” says Gupta.
CanKids is another NGO that includes palliative care for children as a vital part of its care-giving portfolio. “We have set up many sustainable low-cost models of support, including Home Away,” says Poonam Bagai, founder of CanKids and Vice-Chairman of Pallium India. “We have the only pediatric palliative care center in Delhi and a special school in Mumbai for children with cancer, called Canshala.” Bagai, a cancer survivor herself, feels that the programme is strengthened by the presence of a dedicated stream of volunteers.
In Kerala, there are over 300 voluntary groups like the Neighbourhood Network in Palliative Care, which coordinate and network among themselves, besides associating with hospitals and other institutions to help the critically ill.
Volunteers are indeed the backbone of a successful palliative care programme, as the ‘Kerala model’ has unambiguously proven. In Kerala, there are over 300 voluntary groups like the Neighbourhood Network in Palliative Care, which coordinate and network among themselves, besides associating with hospitals and other institutions to help the critically ill. These volunteers provide much-needed home-based care, often as a support to the ongoing medical treatment in order to relieve patients’ suffering and provide physical and emotional support to their families. They also ensure that financially strained families already reeling under the burden that the treatment of a life-threatening illness entails, are provided for, in terms of basic needs, from food to education.
“What has happened in Kerala is beautiful. But it should not be confined to Kerala,” opines Dr. Rajagopal. “Though I trained in radiation oncology, my interest in palliative care largely developed due to my own personal journey of having looked after my mother who was diagnosed with stage 4 cancer,” says Dr. Thomas. “Though there is no cure for advanced-stage cancer, patients do show symptoms which require medical attention. The difficulties I faced despite being a doctor are what led me to think of the need for home-based care and of the vast majority with no medical background.”
Dr Thomas’ organization undertakes house visits to patients, counseling their families and offers medical advice and pain relief treatment in the comfort of the patient’s home. One of the biggest stumbling blocks in India towards making palliative care accessible to the masses was the strict regulation on morphine. Though morphine is quite cost-effective, its use had been restricted heavily in the country since 1985. Due to a perhaps misdirected concern about drug abuse, the country has been regulating the availability of morphine, leading to constrained access to a cheap method of pain relief for millions of terminally ill patients. What’s worse, most of the doctors trained in the country are not conversant with the use of morphine in palliative care.

Dr Boby Sarah Thomas
Founder, Cancare Home
Healthcare Services,
Kerala
Since 1998, palliative care centers in Kerala were allowed to give the drug in oral form to patients. The Centre relaxed the norms for morphine across the country in 2014, allowing freer access to the pain-relieving drug. Dr. Rajagopal, however, feels that changing the law will not translate into practice unless someone pushes its implementation. “The new law has not had a big effect,” he elaborates. “Figures show India uses 320kg of morphine a year. To meet the need we would need to use 30,000kg.”
On the one hand, when advancing standards of medical care have been key in increasing the average lifespan of the Indian population, on the other hand, this means a large-scale shift from acute illnesses to chronic illnesses, which means almost 60 percent of patient deaths in the country are due to chronic illnesses and related suffering. This shift has, in turn, intensified the demand for palliative care in the country, with the number of patients needing it annually being around six million.
Also, considering the expertise and skillset required to deliver palliative care, the field is expected to witness a growth rate of 20-25 percent in the near future. “One of the biggest misconceptions about palliative care is that it is restricted to end-of-life care or to terminally ill cancer patients,” says Dr Rajagopal.
Due to a perhaps misdirected concern about drug abuse, the country has been regulating the availability of morphine, leading to constrained access to a cheap method of pain relief for millions of terminally ill patients.“In reality, palliative care can, and should, be part of the care plan from the time of diagnosis of any chronic or advanced illness. It is care that aims to improve the quality of a patient’s life and that of his/her family through the illness trajectory and even after bereavement. Then there is the awareness and advocacy issue. There are no groups of patients or even families of the terminally ill that can take their case forward. We need a movement to get the government to focus on palliative care.”
Enabling Caregivers
A grave illness does not just affect the patient, but family and friends as well. The patient’s family and network of caregivers need awareness about palliative care, as well as emotional and financial support to get through the harrowing times.

A beneficiary of CanSupport’s counseling sessions, Rashmi explains her struggle when her husband passed away due to cancer. “I was the one who mostly took care of my husband,” says Rashmi. “But being the breadwinner of my household, after his passing, I had no option but to get back to work immediately.
Most days, I felt guilty for not having mourned my husband’s demise, and it took a toll on me. After having shared my story with one of the counselors at CanSupport, I felt relieved, almost as if a huge burden had been taken off of my mind. I was advised to allow myself some time to grieve and focus on myself, after which I felt confident enough to head back to work.”
“SADLY, IN INDIA, WE ONLY LOOK AT THE DISEASE AND ENTIRELY IGNORE THE PERSON. WHAT WE NEED IS NOT JUST DISEASE-CENTRIC TREATMENT BUT AN INDIVIDUALISTIC-FAMILY CENTRED APPROACH TO TREATING A PERSON.”
Dr M R Rajagopal
Chairman, Pallium India

Timely advice and support can change a patient’s experience with illness as well as provide a positive experience to the entire family. Jessy Varghese, whose mother-in-law, Victoria George, 79, lost her battle to lung cancer, says her end-of-life experience would have been far worse had it not been for Dr Thomas’ Cancare. “My mother-in-law was diagnosed with end-stage lung cancer around eight months before she passed away,” says Varghese. “She was already frail by the time the disease was discovered.
The doctors insisted on doing a needle biopsy and were pressing us into doing it. But we were unsure about putting her through more pain, especially when no cure was available. However, we would not have been able to resist the pressure if not for Dr. Thomas. She assured us of our decision to not put our mother through unnecessary trauma during the last days of her life.
We wanted to focus on making her last days the best days ever, and with support from Cancare, we were able to do so. We even had one of the best Christmases ever in 2016, when the entire family got together to be with her. She passed away a month later, and we believe that helping her be at home rather than in a hospital, helped her pass in a peaceful, more contented manner.” Dr. Thomas shares another story about the unique challenges families face: “One of my patients, a 65-year-old suffering from end-stage liver cancer, lived with his son who was a bank manager. The son had to quit his job as his father required frequent visits to the hospital. Learning about home-based palliative care came as a great relief to the family as transporting the patient to the hospital each time was a huge challenge.”
WHO defines palliative care as care that:
- It provides relief from pain and other distressing symptoms.
- Affirms life and regards dying as a normal process.
- Intends neither to hasten nor postpone death.
- Integrates the psychological and spiritual aspects of patient care.
- Offers a support system to help patients live as actively as possible until death.
- It offers a support system to help the family cope during the patients’ illness and in their own bereavement.
- Uses a team approach to address the needs of patients and their families, including bereavement counseling, if indicated;
- Will enhance the quality of life, and may also positively influence the course of illness.
- Is applicable early in the course of illness, in conjunction with other therapies that are intended to prolong life, such as chemotherapy or radiation therapy, and includes those investigations needed to better understand and manage distressing clinical complications.
WHO’s definition of palliative care for children:
- Palliative care for children is the active total care of the child’s body, mind, and spirit, and also involves giving support to the family.
- It begins when the illness is diagnosed and continues regardless of whether or not a child receives treatment directed at the disease.
- Health providers must evaluate and alleviate a child’s physical, psychological, and social distress.
- Effective palliative care requires a broad multidisciplinary approach that includes the family and makes use of available community resources; it can be successfully implemented even if resources are limited.
- It can be provided in tertiary care facilities, in community health centers and even in children’s homes.
The Grim Facts
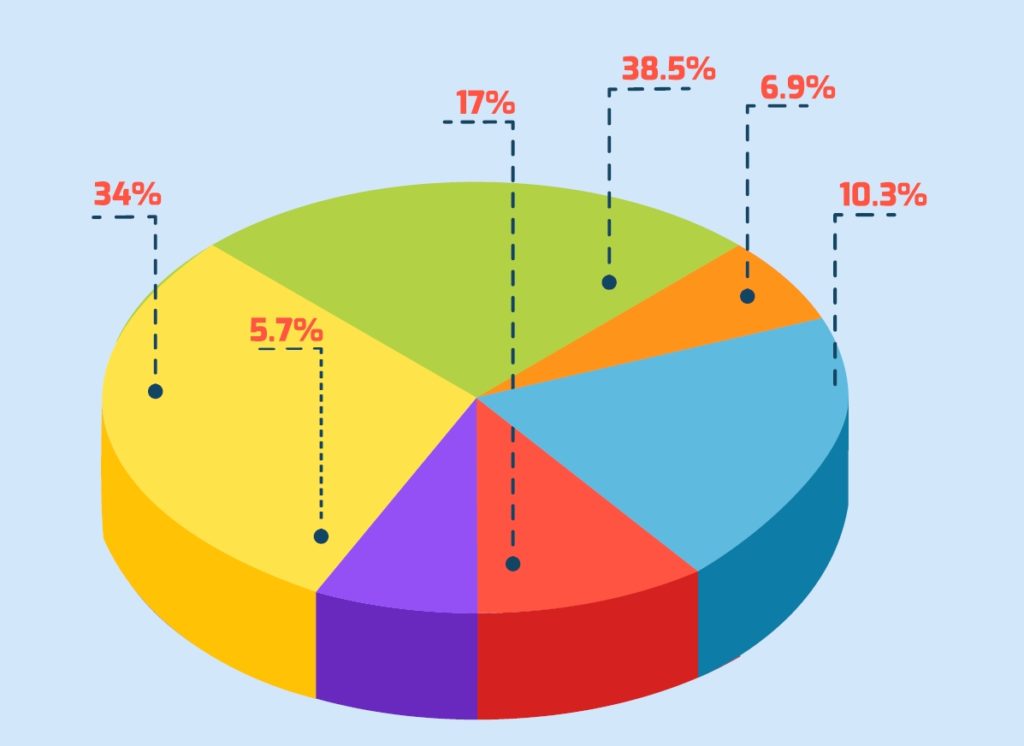
Most adults need palliative care for chronic diseases like cardiovascular diseases (38.5%), cancer (34%), chronic respiratory diseases (10.3%), AIDS (5.7%) and diabetes (4.6%). Other conditions that require palliative care: kidney failure, chronic liver disease, multiple sclerosis, Parkinson’s disease, rheumatoid arthritis, neurological disease, dementia, congenital anomalies, and drug-resistant tuberculosis.
National Palliative Care Strategy

First ever global resolution on
palliative care adopted
- Introduced in 2012
- To create basic palliative care infrastructure across India
- Was to be implemented in the five-year plan ending 2017
- However, it was not funded
- Centre sets up Flexi pool for states to avail funds
- States could use up to Rs 48 lakh to set up 10-bed district palliative care centers
- Funds claimed only by Kerala, Maharashtra and Tamil Nadu so far
Progress Towards Solace
After repeated efforts led by Pallium India and other concerned organizations, the Medical Council of India (MCI) has included palliative care as a specialty and has introduced a postgraduate course for the same. “It is needed in undergraduate education too,” argues Dr. Rajagopal. “Medical students today find it difficult to assess and manage pain as the focus is increasingly on the disease.” But the move by the MCI is still a ray of hope and an indicator of progressive change that is sweeping across the country.
The Delhi government is considering setting up palliative care units in every major hospital that falls under its aegis. The state health department is focused on bringing palliative care closer home to patients, especially to those afflicted by cancer, and plans to train doctors, nurses, paramedical staff and even technicians on the basics of palliative care.
As renowned cancer specialist Dr. Robert Buckman once said, “If you aren’t able to communicate with your patients, you can’t find out how bad their pain is. And if you can’t find out how bad their pain is, there is zero chance of your being able to relieve it effectively.” In India, the dialogue has finally begun towards enabling palliative care for every single patient in need.
Why palliative care?
You are a bridge. When you’re healthy, when the bridge is sound, you can handle anything, all the oncoming traffic of life. But if you’re facing a serious health issue, like cancer, Alzheimer’s or heart disease, the bridge starts to falter. Slowly it becomes hard to withstand all the traffic, traffic that includes your medical treatment. And that’s where palliative care comes in. A specialized form of medical care specifically designed for people with serious illnesses, its main goal is to improve your quality of life by providing relief from the symptoms, stress, and pain that are inevitable byproducts of both the disease and the medical interventions. In other words, palliative care is the support your bridge needs.
Just like construction, palliative care is a team effort. It takes doctors, nurses, carers, social workers, and other specialists, all working together with your physician to provide that extra layer of support—the layer of support that will make all the difference to your bridge. One that can be provided along with curative treatment, palliative care is a treatment method that makes sense at any stage of an illness or at any stage of life, because it’s never too late to lessen the burden. In the future, if you or a loved one is facing a serious illness, remember this bridge analogy, and be sure to consider the immense potential of palliative care in bettering people’s lives.