Multidisciplinary Team in Cancer Management

The importance of getting the right superspecialist on board and availing the services of a Tumour Board
Diseases can be classified into four main types, viz. infectious, deficiency, hereditary, and physiological diseases. Another way of classifying them is communicable versus non-communicable diseases. Cancer is a general word used for a large group of different diseases (more than 200), which have growth of abnormal cells that can invade adjoining parts in the body as well as spread to distant parts. As per the World Health Organization (WHO), cancers are the second leading cause of death worldwide, and caused 9.6 million deaths last year (2018). In fact, they are also responsible for a staggering annual economic cost that was estimated to be more than $1 trillion in 2010. Thus, cancer is part of the growing challenge of non-communicable diseases faced globally, with 70 percent of deaths being concentrated in low- and middle-income countries, like the SAARC region. The real increase in the incidence is also matched by the growing infrastructure to tackle it as well as the willingness of patients to undergo treatment. Being a disease whose incidence increases with age, patients diagnosed with cancer often have significant co-morbidities like diabetes mellitus, hypertension, and arthritis. These are also lifestyle diseases and impact on how patients are assigned as well as tolerate their treatment. Almost one-third of deaths from cancer are directly linked to lifestyle choices—tobacco consumption, obesity, low fruit and vegetable intake, lack of physical activity, and alcohol. Hence, cancer management is best left to professional experts who have the right qualification, experience, and training.
IS CANCER CURABLE?
There is often a lot of skepticism when the word ‘cure’ is used. Some authorities discourage the use of ‘cure’ as a terminology except in limited types of diseases. The main goals of cancer management are to cure, to considerably prolong the life of patients and to ensure the best possible quality of life for cancer survivors. So why is the word ‘cure’ applicable to cancer? For that, we need to look at the WHO definition of the word. A patient is considered cured if the following factors are fulfilled: All evidence of the existence of the disease is now absent.
The person no longer needs medication/ treatment. Life expectancy returns to normal. It is therefore obvious that diseases or illnesses that can be cured will NOT include diabetes mellitus, hypertension or arthritis. Common ones that can be cured will be infections (like pneumonia treated with short-course antibiotics), nutritional anemia (treated with short-course oral haematinics with/ without deworming) and cancer!
“I have got a dream that is worth more than my sleep.”
Vandana Gupta, Survivor, [email protected]
Yes, some cancers are potentially curable, provided they are detected in time and managed correctly. While this may not be applicable to all cancers, the list is growing steadily. Today there are several examples where cancer patients are alive and well 20, 30 and even 40 years after completion of their treatment.

“Patient support groups are the best way of reassuring new patients. When they discuss with ex-patients, they immediately get the confidence to fight cancer positively.”
Sachin Hingmire, Senior Medical Oncologist, Deenanath Mangeshkar Hospital, Pune
THE FIRST CHANCE IS THE BEST CHANCE AGAINST CANCER
In life, we often get a second chance. Not in cancer, however. If there is one thing that the readers must remember from this article, it is the fact that the best chance of benefit from anticancer treatment is the FIRST CHANCE. Cancer treatment should not be commenced unless the diagnosis is certain. However, once it is confirmed, there is a need to develop a systematic care plan and implement it at the earliest. We must also stress the importance of taking the advice of the right specialists. While many patients continue to get treated by general surgeons, internists, family practitioners, and other healthcare providers, remember that the best outcome is when under the care of the right oncologist. For instance, if a patient has ovarian cancer, survival with surgery appears to be higher when a gynecological oncologist performs the surgery compared with a general gynecologist. Because it is only oncologists who remain aware of recent advances, current treatment options and results of clinical trials—so that the best care plan can be developed for your specific cancer. There are also different types of oncologists (See Figure 1). In allopathic medical education, it takes more than six years plus to get the MBBS degree (graduation in the medical field). After that, it takes at least three more years of studies before a postgraduate degree can be obtained (General Surgery, Obstetrics & Gynaecology, Internal Medicine, Radio Therapy/ Radiation Oncology). Radiotherapists, thus, qualify within 9 years of joining a medical college and treat cancer patients by radiation therapy, ably assisted by medical physicists (who calculate the dose of radiation) and technologists.
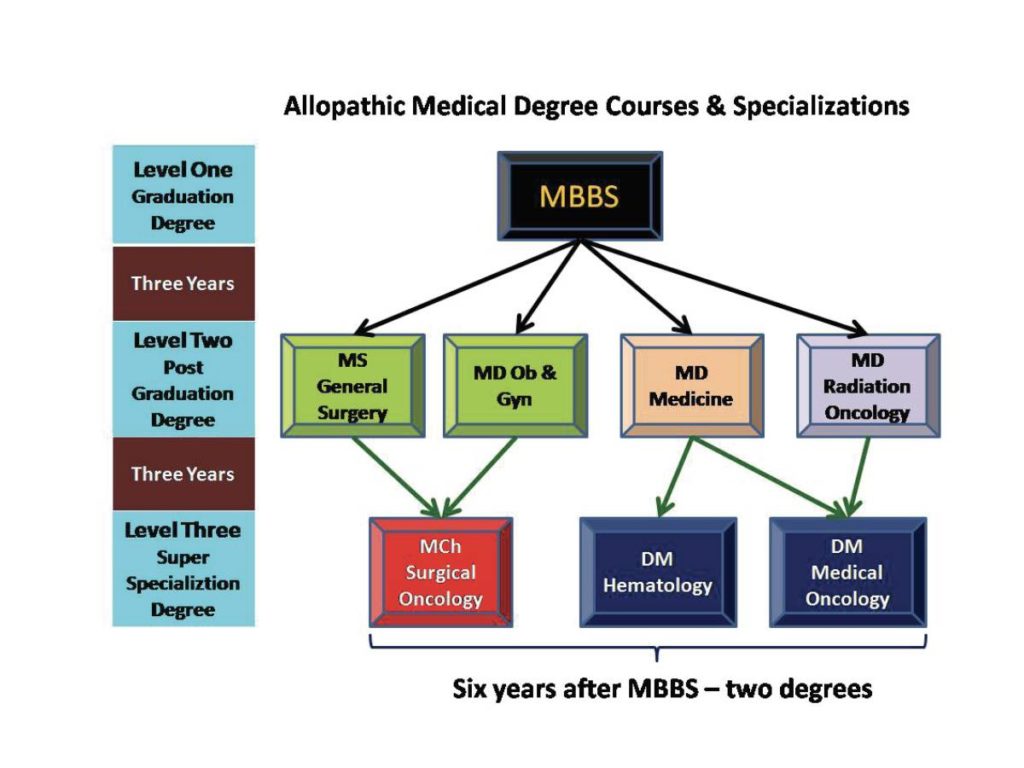
The course for super specialization (MCh. in Surgical Oncology or DM in Medical Oncology/Haematology) requires three additional years. Candidates eligible to be admitted for the course of DM in Medical Oncology include MD in Internal Medicine, Paediatrics or Radiotherapy. MCh. surgical oncologists are ideally-qualified superspecialists to operate on cancer patients and DM medical oncologists are superspecialists entrusted with the task of administering cancer-directed systemic therapy (commonly called chemotherapy). Both MCh. and DM requires a total of 12 years of rigorous training. We interviewed three oncologists from different parts of India who first took MD in Radiotherapy from three of the most prestigious medical teaching institutes in our country: PGI (Postgraduate Institute), Chandigarh, TMH (Tata Memorial Hospital), Mumbai and AIIMS (All India Institute of Medical Sciences), New Delhi. Each of them went on to pursue DM in Medical Oncology at TMH, Mumbai and are currently serving at Patna, Mumbai, and Vizag. We asked them why they chose to do DM in medical oncology after qualifying as MD in RadioTherapy and whether they are happy with their decision. Cancer is a serious illness. So patients should take sufficient time and effort to educate themselves regarding the type of cancer they have, about the oncologists they should consult and about the cancer center where they are comfortable taking their treatment. Talking to other cancer survivors and cancer support groups can also help. Online cancer discussion groups and communities allow asking for frank opinions with the comfort of anonymity.

“After completing MD Radiotherapy, I understood my zeal to learn more in the best interest of my patients. Yes, doing DM in Medical Oncology thereafter was the right decision.”
Dr. Vijay Patil Asst Professor, Dept of Medical Oncology, Tata Memorial Hospital, Mumbai

“I wanted to prove that after completing MD Radiotherapy, I can also work equally hard to get admission into and complete DM in Medical Oncology.”
Dr. Avinash Pandey, Asst Professor and Incharge Dept of Medical Oncology, State Cancer Institute, Indira Gandhi Institute of Medical Sciences, Patna

“After taking admission for DM in Medical Oncology, I worked hard to ensure I got full training in finer points of internal medicine and critical care, skills required to optimize care in chemotherapy administration.”
Dr Sujith Kumar, Specialist Registrar, Homi Bhabha Cancer Hospital & Research Centre, Vizag
All three of them completed DM Medical Oncology super specialisation at Tata Memorial Hospital, Mumbai
Once a decision is made and the treatment plan agreed upon, it is vital to stay committed and to follow it diligently and completely. Patients who drop out of it, delay treatment schedule (e.g. for social reasons) or forget to take medicines regularly do not get the intended benefit. These are the patients who miss out on the best chance of overcoming their cancer. A 10 percent compromise on the dose intensity can lead to as much as a 50 percent reduction in treatment benefit. There could be social reasons why patients and families fail to take treatment on time. For instance, during festivals and agriculture-related (sowing or harvesting) seasons, the number of patients coming to the hospital always reduces significantly. There could also be personal reasons like a family function. Cancer patients must understand that their treatment should get first priority if they want the best chance of getting better. Other seasons, festivals and occasions will come frequently. But the chance of cure is lost forever if the treatment schedule and administration are compromised. Patients have to be conscious of this fact and make a decision on what is more important to them: a patient-centric individual choice. Giving up bad habits or lifestyle choices is equally important. Giving up tobacco (even after the diagnosis of cancer) is known to improve tolerance to therapy and overall survival rates. Diet and inclusion of the right nutrients also play a vital role.
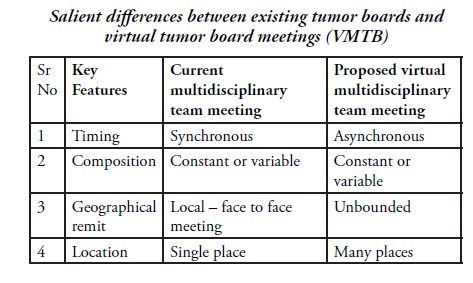
Multidisciplinary team (MTD) and Tumor Board Meetings (TBM)
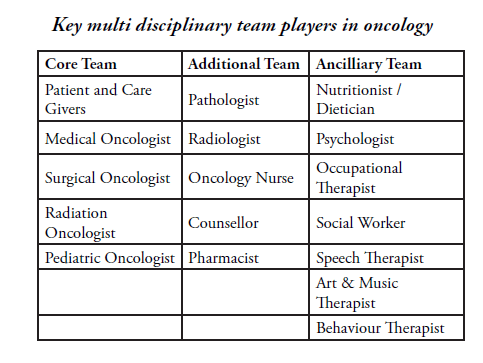
Cancer is the classic example of where a multidisciplinary team(MDT) is extremely useful. The multidisciplinary team includes a group of healthcare professionals from different disciplines, each providing a vital component of the overall services required for the patient. Each team member independently addresses various issues a particular patient may have. In order to coordinate each one’s inputs and arrive at a personalized care plan, the MDT meets in a Tumour Board to discuss patient details. There is ample evidence that such MDT Tumour Boards lead to improved outcomes in cancer patients. This works because each member of the MDT brings his/her own unique qualifications, skills and experiences; it provides the patient with the benefit of the entire team of experts. It also improves service coordination, shortens the time for referral to other specialists, disseminates learning quickly, and identifies gaps in a timely manner. This, of course, requires a lot of time and commitment from the team members to attend such meetings, listen patiently to patient details and then discuss the various treatment options before finalizing the ideal care plan. Patients and their family members remain unaware of the dedication, time and planning required to do this for their benefit. Some of the major benefits include accurate treatment recommendations and adherence to current clinical guidelines. Since a Tumour Board Meeting (face-to-face meeting of several specialists and healthcare professionals) requires all of them to come together at the same time and devote several hours and efforts.

“My cancer treatment at Asian Institute of Medical Sciences has been very successful. The doctors who treated me, Dr Prashant Mehta and Dr. Vinay Gaikwad have excelled in their job. They make a dream team for cancer treatment. The services at the hospital are good. The facilitator, Mr. Arvinder, has been very helpful. I am happy and recommend any patient to this prestigious hospital.”
Somdutt Dulthumun, from Mauritius, with Dr Prashant Mehta

“I was delighted with the facilities of Shably Hospital and the way all the staff treated me during the six months of my chemotherapy. I have been relieved of my disease and my symptoms. I have no tension now.”
Mobin Khan Pathan, from Abu Road, Rajasthan with his oncologist Dr Bhavesh Parekh
Is there an alternative option available? Yes. This is called the virtual Multi-Disciplinary Team/Tumour Board (VMTB). This is especially valuable for rare tumors, when team members are busy elsewhere or where a large number of patients need to be discussed. VMTB is a novel approach that is quickly being valued for its benefits. Allowing asynchronous communication is a feature of the VMTB approach that has been taken advantage of by several organizations, including AFIP, iPath, UICC-TPCC, and Virtual International Pathology Institute. Technical features include the ability to communicate using text-based comments; images with superimposed comments; and short audio or video clips—all uploaded on a web-based system that can be accessed by authorized users in a secure manner from anywhere in the world.
Second Opinion
The other alternative to a TBM or MDT is to obtain second (3rd, 4th or even 5th) opinions. This is valuable when the treatment center does not have all the healthcare professionals required for particular cancer or patient. This is especially useful for community oncology specialists, particularly so if they are from tier 2 and tier 3 areas. When faced with a diagnosis of cancer, patients tend to go through anxiety (and a series of emotions) before coming to terms with it. This may include denial, anger, frustration, resentment, depression, etc. The way forward is for patents to achieve acceptance as soon as possible. A second opinion often plays a vital role in speeding up this process. Some well-meaning family members and friends also insist on a second opinion, especially from oncologists whom they have been impressed with in the past. Patients often hesitate to discuss the desire to take a second opinion, because they do not want to offend their family physician or their oncology specialist. They should not have such concerns. Most doctors understand the need for patients to seek a second opinion. Taking their primary doctor into confidence, and sometimes taking their help to set up the appointment, is the best way forward. In fact, it is important to understand that, when doctors are faced with the diagnosis of cancer, they usually take a second opinion. Oncologists also take an informal second opinion from their colleagues regarding their patients. This is with the intent of providing the best treatment to their patients. This should not be taken as a mark of a lack of confidence or knowledge. It is a common occurrence using smartphones, WhatsApp and social media. In fact, there exist a lot of online groups where specialists take informal advice from their colleagues without charging a single penny to their patients. Turnaround time is quick too.

“After my daughter died of blood cancer, I founded an organization, which caters to the needs of children suffering from long term illness. I named it Solace. For the hundreds of cancer patients that have come to me in the past 20 years, I have approached Dr Purvish Parikh for guidance. When I send him patient details, test reports or any query, he reverts backs with inferences and treatments almost immediately. For me, all through these years, his comments are still the last word.”
Sheeba Ameer, [email protected]

“Education in cancer is a continuous process because there are better medications and modalities of treatment that are available every six months or sooner. By interacting at regular intervals, oncologists get the opportunity to share their experiences, identify unmet needs and brainstorm on how to find the right solution based on the unique needs and preferences of our patients. This is an evolving process and I’m excited about how this benefits the patients by improving outcomes.”
Dr Bharath Rangarajan, Senior Medical Oncologist Kovai Medical Centre & Hospital, Coimbatore

“I have been running a successful business for 12 years. I had the bad habit of consuming tobacco. When I suspected something in my mouth, I went to my family doctor who said it was nothing. After coming back from Kumbh Mela, I realized I had to consult an expert. I was referred to Dr. Purvish Parikh who quickly made the right diagnosis and got me operated. Within a week, I recovered completely. My cancer was diagnosed in stage one. I have given up tobacco for good and will be working with Dr. Parikh and others to spread awareness about oral cancer prevention and early detection.”
Madhusudhanan Menon, from Thane, with Dr Purvish Parikh [email protected]

“We constantly strive to convey the importance of following a healthy lifestyle. Tobacco is the number one cause of cancer. Public awareness about its harmful effects will not only prevent the development of cancer but also several other diseases – of the heart, brain and lungs. The government has banned its use in public places and also mandated huge pictorial warnings on tobacco packs. If our population takes heed, half the cancers would be avoided. This would be a huge benefit for patients, their families and for our nation.”
Dr Prasad Narayanan, Senior Medical Oncologist at Cytecare Hospital, Bengaluru
There are several websites and online resources that are able to provide remote second opinion services from cancer experts. Patients have to carefully make the right choice to obtain the maximum benefit. Some patients are enamored by the western world. Unfortunately, opinions from the USA/Europe are fraught with several flaws. The classic example is IBM Watson for Oncology. The doctors who ‘trained’ the software were all from a single institution on the east coast. Their biases cropped into the computer system and the output from the artificial intelligence was therefore biased too: as they say “garbage in, garbage out”. In fact, many organizations including MD Anderson Cancer Center have given up using IBM Watson because it did not add any benefit at all. Another problem with recommendations from the western world is that they are limited only to the guidelines applicable to them based on insurance reimbursement and will primarily recommend treatments that are licensed by the US FDA. Some of these drugs are not available in countries like India. On the other hand, drugs available in our country, but not licensed in the USA will not be recommended, even if they are of proven benefit. So the best option for a second opinion is to use an online facility available within India where it is possible to get the opinion of several national-level cancer experts at the same time. If five experts agree to the best line of treatment, it is the equivalent of the best brains giving personalized care plans in the best interest of the patient. Such a balanced consensus will be ideal for patients.
Also read about